So, it has been a long time. Many things have happened. That is, in part, why I haven’t updated. I didn’t want to post about the new procedures I was going through until I knew if they were helping at all. I wanted to have some sense of closure. Not as though the closure meant I had finished treatment and no longer felt sick, but that I was stable. It has been only until now, where I feel I have reached that point again.
I apologize in advance, for the long post, but I wanted to get caught up so I can continue with updates more recent.
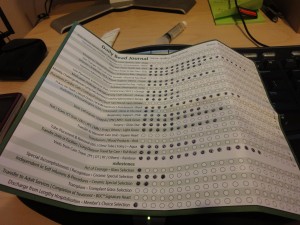
My gastroenterologist (GI) was at a loss when it came to managing my decreasing motility of my large intestine. I had to visit the ER at least once a week due to intolerable pain. The x-rays taken there, all showed the same picture and over time, my doctor was able to see everything over a large time frame. It was then that he realized the severity of my lack of intestinal motility. After we ran out of options he was able to offer, my GI went searching through his co-workers and found my new interventional radiologist (IR), Dr. Osnis. It was then that I was presented with the c-tube treatment plan. This is the first time I had ever heard of a c-tube, or a cecostomy tube, and I usually know quite a bit about all options for any digestive problem now that my motility and paralysis is progressing.
The other posts I have blogged here, show the detail in research I do in order to fully understand the concepts, procedures and the life I would live after starting/completing treatment. I stress the importance of almost obsessive compulsively researching when it comes to your health and illnesses/diseases. You must NEVER put all of your faith and trust into any healthcare professional. After all, they are people too and people make mistakes and they can’t be expected to know everything. Placing medical caretakers on some sort of pedestal can seriously compromise your health and be potentially fatal. An example of this will be given later. Yes, it happened to me very, very recently, through no fault of my own.
I think the last time we all talked was when I was in the middle of attempting to control my lower digestive system with a c-tube, or tube placed in my cecum. Wow, that was way back in August of 2012. So sorry it has been so long. Anyway, it is the same tube concept of a jejunostomy, just placed in a different area (the cecum; the first section of the large intestine). I had a long tube with a continuous drain placed first. As with all other tubes, the longer tube was placed first to establish a healthy tract built up of scar tissue. This assures that the tube, should it become dislodged or otherwise dysfunctional, can be easily replaced. It also helps reduce any pain that might be associated with manipulation or tube movement.
I agreed to the c-tube and had it placed through the standard outpatient procedure associated with any tube placement. At first, the long c-tube attached to a draining bag, was working really well. I was seeing results. The drainage bag was filling with air on a constant basis. This was precisely the purpose for which it was placed. But then, it didn’t seem to be working. I became afraid. I have been here before, the place where you know something is wrong but can’t produce evidence that would support your feeling. I made many visits back to my IR to have the tube checked and each time, it showed the tube to be functioning correctly. They pushed contrast through my tube that would show up on a special type of x-ray. I saw it myself. But when I’m home, nothing comes out of my tube. The draining bag was sutured open. The valve wasn’t broken. Why wasn’t it working?
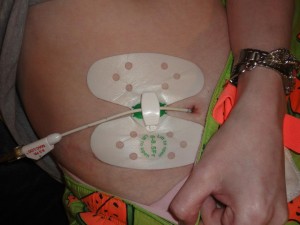


I stopped getting relief that the tube was placed to offer. The tube my IR placed was only a 8.5FR (FR = French, a unit used to measure the size of tubes = How tubes are measured). I didn’t understand why the tube was so small. For as big as my distended colon was (10cm at the biggest!), I felt the tube should have been bigger. Once my tube site and internal tract healed and was strong enough to withstand a tube change, I requested my long tube be switched out for a low-profile tube as well as a larger tube. It took a few weeks for my tube that needed to be specially ordered, to be available for placement. I received a 16FR Mic-key button to replace my 14FR tube. I thought that with a shorter tube in length, on the inside, coupled with a bigger tube, I would find a constant and greater relief in my symptoms. This, I believe, is where I left everyone last time I blogged.

I began my routine from before, visiting the ER every week for abdominal pain. The x-rays looked just as bad as they did in the past. Throwing his arms up in the air out of frustration, my GI referred me to my new colorectal surgeon. This man is amazing. The best bedside manner I have ever experienced. He treats every patient like his own child. This has been said before about so many other physicians but in this case, it is the truth and best way to describe this man. He knew that if my GI, an extremely skilled and knowledgeable doctor, sent me to him that my GI had to be very desperate and concerned. Turns out, my new colorectal surgeon would be the right person to offer the right treatment. Looking back now, I could not be happier with the decision I made to agree to the proposed treatment/procedure.
When I saw my surgeon, Dr. Bastawrous, he told me that he would NEVER suggest a c-tube. He told me that a c-tube is by far the worst idea. I wish he was around when I was having the c-tube placed. I could have bypassed a lot of pain and a few surgeries. He didn’t know. In any case, he said that given all the x-ray images, symptoms and other illnesses, there was really, only one option left. An ileostomy.
There were two different types of ileostomies that we were considering and in the end, I decided to do what was less invasive. An open ileostomy. Exactly what this is, how it works and what different types of ileostomies are available will be discussed in a new section under experiences once I am able to get all the information collected. I think people forget to investigate all possible options when it comes to treatment. They are blind to those treatments that are least invasive. As you can see through my experiences and blogged entries, I started with the least invasive treatments from the very beginning, giving them a fair shot. First I started with simple diet changes. I moved from diet changes to medications to temporary feeding tubes to permanent feeding tubes to PICC lines to ports for TPN to c-tube to ileostomy. As much as the c-tube did not work, it was still worth my time to investigate and in some instances, try. Even the type of ileostomy I have isn’t exactly permanent. In some future situation where I begin to regain the ability to eat orally, my ileostomy can be reversed. While that isn’t likely to happen, taking out all of my large intestine is a huge shock to the body anyway. Leaving it in place makes sense and being able to reverse it is just a bonus.
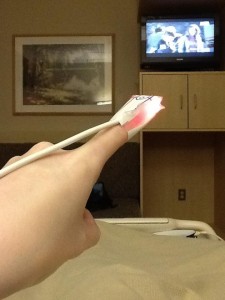
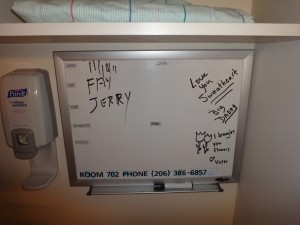
Come October, I was taken in for an ileostomy surgery where my c-tube was also reversed during that time. My appendix along with the cecum of my large intestine was removed and the stoma for my ileostomy created. My large intestine was completely physically disconnected from any of my organs. Nothing was allowed to go through it. Everything was to come through my ileostomy. It was a very large shock to my life. I thought I was prepared through all the research I did and conversations I had with other patients that had already had an ileostomy done. But the truth is, you can’t be completely prepared for something that is to change your lifestyle forever. Usually the surgery puts you in the hospital for around 3 days. I had some complications that kept me there for over five. The pain was controlled and honestly, the pain wasn’t very high given the procedure that is done. You know, a large hole in your abdomen that is kept open with part of your small intestine pulled through. Yeah, things will hurt for awhile. Any surgery comes with pain. Sometimes you just have to knuckle-down and take it.





Thanks goes out to the many GP friends I met through Facebook, that came to visit me while inpatient for my ileostomy. Thanks go out to everyone who continue to offer encouraging words. You guys rock! I love you all! We must get together again. Preferably NOT in the hospital =)
Once the shock phase ended, I’ve been living with my open ileostomy since then. Like I said before, it was one of the best decisions I have made and that has been presented to me. That is, beside my port and TPN that saved my life and allowed me to get to an acceptable weight (with any illness or procedure, my weight drops back down into the red zone) and stable health. I haven’t had ANY complications, infections or pain in or around my stoma/ileostomy. Aside from a few leakage problems that were due to products that weren’t right for me, I’ve been living relatively comfortably. The products that I have found to be best for me, are the ones made by COLOPLAST. I’ve tried all of the HOLLISTER products (one-pieces and two pieces with their associated pastes and putty) with no success. All hospitals that I’ve been to have only offered Hollister products because they are not a financial burden (e.g. cheap). Once I got home, my HHC that is in charge of my ostomy orders, supplied me with Coloplast products.
I wear a two-piece system with a one-click bag that locks on to the wafer or backing. I required a specific setup because of the location of my ostomy site. I have that gastric neurostimulator still. The battery was recently replaced back in February 2013. The battery sticks out of my abdomen. You can see it and also feel it. I didn’t know for sure, if the ileostomy could even be done because of the location of the stoma and the location of my battery for the gastric neurostimulator. Somehow my surgeon, the amazing colorectal surgeon, was able to maneuver around my battery in order to safely perform the ileostomy. Even still, the stoma is very close to the location of my battery making any ostomy bag system difficult to stick to my skin and form a tight seal in order to prevent leakages. It took me a few months to figure out the right placement, the right wafer size and the use of other products to keep in what vents out of my ileostomy. Ever since then, I’ve not experienced any problems with my ileostomy (or anything associated with my ileostomy).
My ileostomy is doing what we all hoped it would; vent gas and material that would otherwise obstruct my large intestine until the pain was so intense I required an ER visit and at times, hospital stays. Random imaging studies confirmed the success of my ileostomy procedure. And for that, I’m grateful. One thing that keeps me out of the hospital is well worth it. The hospital can help me but sometimes, it can hurt me. With a weakened immune system and nurses who do not practice correct sterile practices when it comes to my central lines, hospitals can be dangerous. Even standard and simple outpatient procedures/surgeries have me needing observation in the hospital but I am sent home in order to not make me more ill.
Fast forwarding through the last months of the year 2012, we come to the end of January/beginning of February and I notice a dramatic increase in my level of nausea. A quick gastric neurostimulator interrogation showed the battery to be completely, 100% dead. My GI was just as shocked as I upon finding this information. It should have lasted a lot longer. My stimulator was set at the maximum settings, so we attributed the draining of my battery to be so quick. In order to get my stimulator back working again, I had to undergo an outpatient surgery to have the current battery switched out for a new one. My surgeon went through his original incision to place the battery and I was sent home the same day with very little discomfort and pain. Much like the first time I had the stimulator placed.
Pictures from my first surgery to place my gastric neurostimulator:



Not soon after my neurostimulator battery was replaced, I went back into severe septic shock. I ended up going to Evergreen Hospital through the ER. I had to go to Evergreen because it was the closest and didn’t require an ambulance ride to get there. Evergreen wasn’t my first choice of hospitals to stay in due to previous experiences in the ER, but I wouldn’t have survived a longer trip. As with all other situations involving sepsis and septic shock, I was very much unaware of how sick I really was and can’t remember what happened during the long hospital stay. I am always better off in the end, anyway. The seriousness that comes with sepsis is very real. You are in danger of not making it through another day. The ignorance you experience truly is bliss.
For those who have never been in such dire circumstances must know a few things:
1. Those who appear unconscious can in fact, hear you.
2. Those who appear unconscious also know when you are with them.
3. When those who are close to death do not feel pain.
4. Those who are close to death experience peace that cannot be achieved anywhere else on Earth.
I know these things to be true from when I have been in a situation where I was unconscious and close to death. I heard my doctors and family when they were around. I knew what they were saying about me even though I was unable to see them or communicate with them. I felt a sense of peace that made me unafraid of what might happen next. I was literally a breath away from death and it was in that moment, in that choice, where I had to decide my future. In my level of unconsciousness I heard my nurses ask me to breathe. Having zero desire nor the feeling of need to breathe, I was not afraid should I choose not to breathe. My job here on Earth was not finished; I took a breath. It was at that moment where I left death behind and never returned. This happens each time I’ve gone septic. It is no joke.
The sepsis I experienced shortly after my neurostimulator battery replacement surgery was due to a urinary tract infection (a result of a neurogenic bladder) that went riding through my blood and made its way to my lungs where it settled and caused serious pneumonia. Because it was not based in my port-a-cath, Evergreen doctors and nurses were able to save my port. They added a jugular PICC line with three lumen to use along with my port-a-cath lines in order to infuse a wide variety of antibiotics, fluids, TPN, pain medications, sedation medications, etc. My jugular line was placed bedside while in the ICU. During the first placement, it did not land where it should have landed. After an x-ray confirmed this, I had to undergo a second line placement on the other side of my neck, in the second jugular vein. This time, it found the right way to my heart. I remained in the ICU for a few weeks and finished out my time there on the main floor. Evergreen Hospital was super good to me. I couldn’t have asked for better nurses and hospitalists. I was lucky. They saved my life. A life that has been threatened a few times before.


After my sepsis attack in February, I found myself yet again in the hospital in the beginning of March. The reason for my stay this time is very private and that is really all I want to say about it. If you are having serious problems getting control over your symptoms, send me a message and I can give you another thing to try.


Now I have been placed within a “care circle.” Basically all of my doctors across two of my hospitals came together to discuss my treatments, illnesses and concerns. The goal of this care group was to have one person who would receive all discharge notes, referrals and charts. This allows all doctors to be on the same page when it comes to treatment. Everyone is aware of what everyone else is doing. My new PCP and her nurse took on the challenge to be that person; the person who will manage the actions of all doctors and nurses, both in clinics and through my HHC (home-health company). My PCP belongs to VM (Virginia Mason). My neurologist, cardiologist, hematologist and gastric neurostimulator surgeon all also belong to Virginia Mason (VM). My gastroenterologist of five years and counting, second neurologist, colorectal and general surgeon, pain specialist, and interventional radiologist all belong to Swedish Medical. Swedish Medical Issaquah is considered my “home hospital.”
My latest hospital stay and septic shock episode involves both of these hospital systems. One day not long ago, I noticed my port site to be extremely sore. It is never sore; so I called my HHC (Walgreens Infusion and Respiratory Services) to talk to the IV nurse on call. The nurse I later talked with wanted to come over and check the port site and see if it needed to be re-accessed. Given the amount of pain I was in, the size of my port, the fact that my nurses had to use the same hole to access the port each and every time because it was so small, my nurse did not feel comfortable re-accessing and urged me to call my doctors in the morning to see if they could check it out. The only person I was able to get a hold of that day was my PCP nurse. She suggested that I come in to see her IV nurse for opinion. I did and that nurse suggested I have a new port placed. Following their judgment, I had a PICC line placed for use while I waited for a new port surgery the following Monday. Monday came and I went into surgery at VM for a new port. This was the first time I’d be getting a port from a surgeon at VM (Dr. Neuzil). My last ports were placed by a physician at Swedish. I assumed the surgeon at VM knew what he was doing.
I went home and all night I was in an amazing amount of pain. I’ve had MANY ports before and none hurt like this. I thought maybe I was just being a baby, so I took some Advil and went to bed. I woke up that night more times than I could count. I woke up out of pain. When my husband woke up, I desperately asked for an ice pack, pain medication and my normal medications. I expressed my level of pain to him, but there wasn’t much he could do at the time. After several hours of no relief, I began taking my temperature. I watched as it increased from 101 to 102 to a high 104.3. I started calling all of my doctors and HHC nurses. No one was in the office. Not one person from my “care conference.” I tried to do things by the book. I finally got in contact with my surgeon’s office after my anesthesiologist from the day before, called as per routine. I called his office right away for direction. I didn’t want to call my husband out of work in the off chance the ER would write me off, wasting my husband’s work day. I didn’t have many friends in town. The desk clerk at my surgeon’s office gave medical advice without question, all of which was completely and absolutely wrong. Out of frustration, I called a friend as a last resort for a ride to the Emergency Room at Swedish – Redmond. I still measured at a 104 in the ER and so they administered the first dose of my IV antibiotic, sent a picture of my angry port site to my IR at Issaquah and administered Tylenol in hopes that it would reduce my temperature.
Here is the picture I took of my very angry and contaminated unaccessed port-a-cath site before I had it removed via emergency surgery at my home hospital:

There was question as to whether or not I should go to the hospital that did the initial surgery. Of course I didn’t feel comfortable going back. With my port being infected not 24 hours after placement only meant one thing; it was contaminated before it was even placed. My hospitalists all told me that in their 30 years of being a doctor, they’ve never seen something like that happen. Well, I guess I’m just lucky! As soon as I arrived at the hospital, I was wheeled back into the OR for the emergency surgical removal of my new port. My anesthesiologist and IR team where there waiting for me way after hours. They were amazing. I came out of surgery with one very large hole in my chest where the port and some unhealthy tissue was removed. The hole was so deep you could slip in a whole silver dollar. It also hurt like nothing else I’ve felt. The wound was packed and then dressed with a wet to dry dressing many times a day. I remained in the hospital for a few weeks. Once the contaminated port was removed and sent out for testing, my temperature broke and I began feeling better.
I returned home to continue treatment with a new company, Providence Healthcare, for wound care where they would dress, pack, and re-dress my wound every to every other day. I won’t go into detail but this activity was extremely painful and slow.
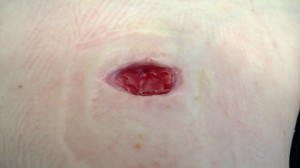

My deep wound could not be sewn up in fear of trapping in even the most common of skin bacteria. This would surely cause the formation of an abscess and that would be entirely counter-productive. I also went home on IV antibiotics, as is usual for sepsis discharge. A month after I finished my IV antibiotics, I would be able to have a new surgery to replace my last two ports. This was done just last Tuesday. I was referred to a new surgeon by my GI doctor. He, Dr. Plaskon, is a general surgeon. He also has wonderful bedside manner. I never lost trust in his abilities as a surgeon. I knew I’d be going into surgery with an open wound, that same open wound that nearly killed me. I was still afraid I would have infection problems with my greatly increased risk of infection from my last few surgeries and open wound. I was set to have my port surgery a few weeks back but they delayed it by a week to allow for more healing of my wound. So Tuesday, May 14th, was the vindicating surgery day where I would attempt to, with the help of my surgeon, fix all that was taken from me a month ago. I wanted to forget. I wanted to erase the day that the VM surgeon nearly took my life through his ignorance and lack of skill. He set my progress back by so much, but I couldn’t let it keep me there.
I was just discharged from my wound home healthcare. My wound has closed. It is scabbed and will leave a large ugly scar. But, scars are like badges of honor received after fighting for your life. I will miss my wonderful wound care nurses. They did everything they could to ensure my wound would safely heal and that I was mentally and physically comfortable. They went above and beyond anything I could have asked for when it came to something so scary as my open wound. They were always in constant contact with all doctors involved and even helped me get the relief I needed when I experienced pain. Ever since my Tuesday surgery, I’ve been extremely emotionally sensitive. I truly appreciate every day given to me and everyone in it. I’m frustrated with my lack of energy and how I’m still restricted by that energy. If I push myself beyond the invisible line my body has, I crash. I become sick. I experience intense migraines. I want to sleep but can’t. So I just hope. Sometimes that’s all you can do. Hope to sleep; hope to live; hope for consolation that needs to come.