Christmas morning landed me in the ER at the closest hospital (which unfortunately happened to be Evergreen – I do not recommend this hospital if you actually want to ever leave in a timely manner) due to fluid retention from the previous day’s fluid infusion. When I came in however, my bloodwork wasn’t quite right, I was underweight, dehydrated and malnutritioned. They also did a CT scan with contrast, when I arrived, showing dilated loops of bowel, suggesting blockage. It was then they diagnosed me with CIP:
Intestinal pseudo-obstruction (false blockage) is a condition that causes symptoms like those of a bowel obstruction (blockage). But when the intestines are examined, no obstruction is found. A problem in how the muscles and nerves in the intestines work causes the symptoms.
Pseudo-obstruction symptoms include cramps, stomach pain, nausea, vomiting, bloating, fewer bowel movements than usual, and loose stools. Over time, pseudo-obstruction can cause bacterial infections, malnutrition, and muscle problems in other parts of the body. Some people also have bladder problems. (Inspire Support Group)
Well good, a new diagnosis that seemed to help me understand a bit more as to why sometimes I had difficulty feeding through my J-tube. I thought my motility problems were only in my stomach, come to find out – they also involved the rest of my intestinal tract as well. Great! Knowing is better than not knowing in this case, I suppose.

So new diagnosis + old diagnosis + newly inserted Picc for TPN…Set me up, sign me out – I’m ready to go home. I knew that chronic illnesses like GP aren’t cured in the hospital, if at all, just managed so I was expecting them to patch me up and sent me home. NOT the case. They seemed to want to keep me there as sort of a project, an experiment if you will. They were not at all familiar with GP or CIP and were working off a day by day plan. I was lucky to see my doctors each day by 6pm if at all. The hospital was beautiful and the nurses were nice and the doctors seemed knowledgable but the management was HORRIBLE. Let’s just say I won’t be going there again. However, late at night – their understaffed hospital allowed us to sneak in my 70lbs Bernese Mountain Dog puppy, Ellie to visit. Pets make everything feel better in ways doctors and nurses never can.
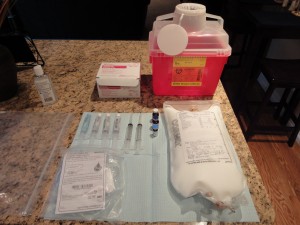
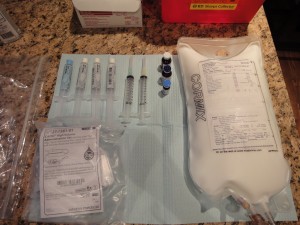
After I had enough of their poking and prodding with no results to show for it, I called Dr. Patterson (whom they had not even contacted during my entire hospital stay) and told him what was going on. I asked him if it was ok if he talk to the hospitalist GI, and he agreed. A few minutes later, she walked in and told me I’d be ok to go home the following day on TPN. I felt sort of bad because I knew they wanted to help solve my problems so badly and I knew they couldn’t. But I was ready to go home. I already missed Christmas and a snow storm…yeah, I was ready. So December 31, 2010 I was discharged from Evergreen Hospital, never to return again.



I made it about a week at home before pain started kicking up to levels that were far beyond my capability to control them. With the CIP diagnosis and GP, Dr. Patterson took me off all pain medication leaving me with only Tylenol. Haha, yeah – that’s going to help. Maybe if I took the whole bottle at once, it might take the edge off enough to walk. I promptly called up Virginia Mason (my comfort zone) and asked for the doctor on call. Who do I get but my Interventional Radiologist, Dr. Siegal. I told him I was experiencing excruciating and debilitating pain in and around my j-tube that radiated to all parts of my abdomen to the point of not being able to use it for the past several weeks. He advised me to come in to the ER and see what could be done. My wonderful husband took me to the VM hospital 30 minutes away. There they drew blood and tested urine and blood pressure. My blood levels came back abnormal, such that they could not let me leave. I was admitted again on the 8th of January. I was given Dilaudid, sleeping medicine (as by this time, it was quite late), and slept it all off.
Early morning my doctors did their rounds. I was not used to this. Doctors? You mean, I don’t have to beg for them to come see me and they are actually here before 6pm?! WHAT IS THIS PLACE. I love you VM. My potassium levels were low, hematocrit was really low, dehydrated and still malnourished. Basically, I felt like crap. The dilaudid was wonderful in controlling the abdominal pain and the rolling migraine that seemed to keep me company during my ENTIRE stay. With low hematocrit levels, they felt I might be bleeding within my intestinal tract (reason for pain). They scheduled me for a colonoscopy and endoscopy for the next morning. Yep, that also meant I had to do the prep. Why? Don’t know. But I did it. I put it through my tube and too fast apparently as it backed up into my stomach and eventually I puked it all back up. Not just the clear GoLytely, but stool. Yeah, not pleasant. Determined, I got the rest of that gallon down and had a successful couple of scopes with normal results. Unsure of where the bleeding was coming from, they simply infused me with iron.
Since VM is the hospital Dr. Patterson left for Swedish, they know him well and they know that I still see him as my GI. My main concerns after my blood levels were stabilized somewhat, was the abdominal pain. They were not going to even go there. I told them Dr. Patterson said to pull the tube and they are like…”We’ll just let him do it.” So I was released on the 12th of February after getting stabilized and saw Dr. Patterson the next day.
When I went in to see Dr. Patterson after being discharged, I was still in considerable amount of pain. He gave me two options: take the whole tube out or deflate the balloon and see if it is just the balloon that is causing the pain while taping the rest of the tube to the outside of your body. I was not a fan of option 2. He sent me for x-rays anyway. After thinking about it that night, I called him and told him I just want the tube out. It was a hard decision as it took so much work just to get it in. But it caused too much pain and I wasn’t even using it, it wouldn’t be logical to keep it in.
He told me to see my PCP and ask her opinion and have her look at it and have her draw some blood. So I did but she didn’t change my mind. My mom was in town but she left early early Sunday morning so I wanted the last day, Saturday to be free from medical stuff, appointments and hospitals, even if I was in pain – I’d have a smile on my face.
Once she left (1/16/11), my husband took me to Swedish’s ER where I told them everything stated here and luckily they found Dr. Patterson and luckily Dr. Patterson (still new to the building) found me. I told him to take it out. It was already extremely painful so I knew him taking it out would just suck even more and it did. As soon as it came out, he knew where most of my pain was coming from. When my button was put in, the tube part wasn’t cut short enough. It ran through nearly all of my lower small intestine and because it was so big, it would nearly immobilize it. When it needed to move to push food through – that’s when it hurt. Plus the button itself got stuck between my ribs so whenever I would breathe or when my intestines moved, it would pull on that button causing waves of pain. So it is better out. Maybe down the road, I’ll be able to get another placed – we’ll just have to see.
So that is my little story as to why I haven’t updated in awhile. I just found some time and energy to put this up and even this took a few days. And in those few days my line might have become infected putting me back in the hospital. Happy thoughts! I hope everyone is having a good tummy day and thank you for your thoughts and prayers!